Explore the science, methods, ethics, success rates, and legalities of gender selection. Essential reading for understanding this complex topic.In vitro fertilization (IVF) has transformed the possibilities within reproductive technology, and among its capabilities is gender selection. This practice, while offering prospective parents the choice of a desired gender, raises a spectrum of scientific, ethical, and legal considerations. In this blog post, we will delve into the scientific principles and methods driving gender selection, from the basics of genetic determination to the latest advancements in reproductive technologies. Furthermore, we will explore the moral debates and ethical implications that accompany the decision to select a child’s gender before confronting the variety of success rates offered by different techniques. Finally, we will review the legal landscape across various jurisdictions, shedding light on where and how these practices are governed by law. Join us as we navigate the intricate world of IVF and gender selection, an area as controversial as it is fascinating.
The Science Behind Gender Selection
Gender selection, also known as sex selection, is a scientific process used to choose the sex of an offspring through various medical techniques. This practice has garnered considerable attention due to its ethical, legal, and social implications. The science behind gender selection primarily involves two main methodologies: Preimplantation Genetic Diagnosis (PGD) combined with In Vitro Fertilization (IVF), and sperm sorting.
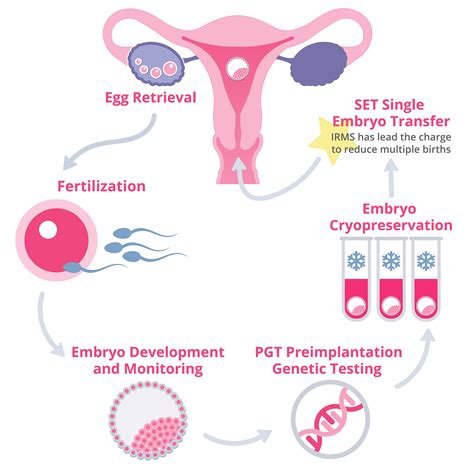
Preimplantation Genetic Diagnosis (PGD) with In Vitro Fertilization (IVF) is one of the most reliable methods for gender selection. It starts with the usual process of IVF that involves hormone therapies to stimulate the ovaries, egg retrieval, and fertilization of the eggs in a laboratory. After fertilization, the embryos are allowed to develop for a few days. Then, a small number of cells are removed from each embryo and analyzed for genetic conditions and sex chromosomes. Only embryos of the desired sex are then implanted in the uterus.
Another method involves sperm sorting, which separates X-chromosome (female) and Y-chromosome (male) bearing sperm through a flow cytometry device. The sorted sperm is then used for either Intrauterine Insemination (IUI) or IVF. This technique is known as MicroSort, but it is generally less effective than PGD with IVF in terms of achieving pregnancy and specific gender selection.
Despite the technological advancements in these methods, the debate around the ethical considerations and legal standing of gender selection continues. Countries vary widely in their regulations and acceptance of these procedures, often reflecting broader societal values and ethical frameworks.
Methods of Gender Selection
In the broad field of reproductive technologies, gender selection refers to procedures used to choose the sex of an offspring. The reasons for this choice can range from cultural preferences to avoiding sex-linked genetic diseases. Here are some common methods currently used for gender selection:
Preimplantation Genetic Diagnosis (PGD) with In Vitro Fertilization (IVF)
One of the most effective methods involves using IVF combined with PGD. After retrieving and fertilizing the eggs, a few cells are removed from each embryo. These cells are tested for both genetic disorders and chromosomal information to determine the sex of the embryo. Only embryos of the desired sex are then implanted into the uterus.
Sperm Sorting
This method involves separating sperm that carry the Y chromosome (which results in male offspring) from those carrying the X chromosome (leading to female offspring). One of the popular technologies used for sperm sorting is called flow cytometry, which differentiates sperm based on the amount of DNA each contains. Sperm with the Y chromosome contain slightly less DNA than those with the X chromosome.
Ericsson Method
Another sorting technique is the Ericsson method, which uses a protein gradient to separate sperm cells by their ability to swim. It is believed that Y chromosome sperm swim faster than X chromosome sperm. This method, however, offers lower accuracy compared to other techniques like PGD.
The choice of method for gender selection can significantly impact its effectiveness and ethical considerations. As such, it is crucial to consult with medical professionals and consider all perspectives before proceeding.
Ethical Considerations in Gender Selection
The debate on the ethical considerations in gender selection is multifaceted, involving a complex interplay of moral, social, and medical factors. The practice of selecting a baby’s sex, often through methods such as Preimplantation Genetic Diagnosis (PGD) used in conjunction with In Vitro Fertilization (IVF), raises significant ethical questions.
One of the primary ethical concerns is the potential for gender imbalance. Predominant preference for one gender over another in certain cultures can lead to societal imbalances and can exacerbate gender discrimination. Proponents argue that gender selection can be a part of family balancing preferences, but critics warn about the implications of altering the natural sex ratio.
Aside from societal impacts, the right to autonomy plays a major role in discussions about gender selection. Some believe that parents should have the liberty to choose the sex of their offspring as part of reproductive freedom. Others argue that such choices place unnecessary value on gender, potentially leading to commodification and instrumentalization of human life.
Medical ethics also come into play in the implementation of gender selection technologies. The use of medical resources for non-medical reasons such as gender preference is often questioned, particularly when there are myriad significant health conditions that lack adequate research funding or treatments.
Further complicating the ethical landscape are the varying laws and regulations about gender selection across the world. This legal disparity not only affects accessibility but also raises concerns about reproductive tourism, where individuals may travel to other countries where the legal restrictions differ significantly from their own.
Ultimately, the ethical debate on gender selection requires a careful consideration of the long-term social, cultural, and ethical consequences of allowing the choice of a baby’s gender in a medical context. Experts, ethicists, and society at large continue to explore these implications to navigate this complex moral terrain.
Success Rates of Gender Selection
Gender selection technologies have advanced significantly over the past few decades, offering various methods to families and individuals who have preferences or medical reasons for choosing the sex of their child. The success rates of gender selection can vary greatly depending on the method used. Herein, we’ll explore how effective these technologies are in achieving the desired gender.
One of the most commonly used techniques for gender selection is Pre-implantation Genetic Diagnosis (PGD) combined with In Vitro Fertilization (IVF). This method involves extracting one or more cells from an IVF embryo to test for genetic conditions and the sex of the embryo. The success rate of achieving a pregnancy using IVF with PGD is largely dependent on the mother’s age and overall fertility health but is widely regarded as highly effective for selecting gender, with accuracy rates approaching 99%.
Another method involves sperm sorting, which separates sperm cells into those more likely to produce male offspring and those more likely to produce female offspring. Technologies such as MicroSort use flow cytometry to sort sperm cells based on the amount of DNA they contain. However, the success rates for sperm sorting are slightly lower than those of PGD, typically ranging from 85% to 90% for females and 73% to 85% for males.
It is important for prospective parents to consult with fertility specialists to understand the potential success rates and decide which method aligns best with their expectations and ethical considerations. Although these technologies offer significant possibilities, they are not without their limitations and potential risks, which must be carefully weighed.
Legal Regulations on Gender Selection
Legal regulations on gender selection vary significantly from one country to another, reflecting diverse ethical, cultural, and social norms. In some regions, the practice of choosing a baby’s gender is heavily regulated to prevent gender imbalances and discrimination, while in others, it may be allowed under certain conditions.
In the United States, there are no federal laws specifically addressing gender selection through reproductive technologies. However, clinics and practitioners often follow guidelines set by professional organizations such as the American Society for Reproductive Medicine, which recommends gender selection only for the purposes of avoiding sex-linked genetic diseases.
Conversely, countries like China and India have strict regulations due to historical concerns over gender imbalance. Both nations have implemented policies that prohibit the use of medical technologies for the purpose of gender selection purely based on family balancing or personal preference.
In Europe, the legal stance varies; for example, the UK’s Human Fertilisation and Embryology Authority permits gender selection only for medical reasons, such as when a child could be born with a serious genetic condition. Similar restrictive measures are seen in Canada, where the Assisted Human Reproduction Act governs the use of assisted reproductive technologies, including those used for gender selection.
It’s crucial for prospective parents considering gender selection to consult local laws and regulations to understand what is legally permissible in their country or region regarding this sensitive aspect of fertility treatments.
Frequently Asked Questions
What is In Vitro Fertilization (IVF)?
In Vitro Fertilization (IVF) is a medical procedure where an egg is fertilized by sperm outside the body, typically in a laboratory environment. The resulting embryos are then transferred to the uterus with the aim of establishing a successful pregnancy.
How is gender selection performed during IVF?
Gender selection during IVF is typically performed using a technique called Preimplantation Genetic Diagnosis (PGD). This involves screening embryos for genetic traits, including gender, before implanting them in the uterus. Through PGD, only embryos of the desired sex are selected for implantation.
Is gender selection legal in all countries?
No, the legality of gender selection varies widely from country to country. While some countries allow gender selection for medical reasons, such as preventing gender-linked genetic disorders, others may restrict or completely ban the practice for non-medical reasons.
What ethical concerns are associated with IVF and gender selection?
Ethical concerns include the potential for gender imbalance, discrimination, and the commodification of human life. There is also a debate about whether parents should have the right to choose the sex of their child purely based on personal preference.
What are the success rates of IVF with gender selection?
The success rates of IVF with gender selection largely depend on several factors, including the age of the woman, the quality of the embryos, and the specific techniques used. Generally, the success rates can vary but are often similar to those of regular IVF procedures.
Are there alternatives to IVF for gender selection?
Few alternatives exist if the goal is to guarantee a specific gender before conception. The most commonly discussed alternative is sperm sorting, which involves separating X-bearing sperm from Y-bearing sperm to increase the chances of conceiving a desired gender. However, this method is less reliable than PGD with IVF.
What should potential parents consider before opting for IVF with gender selection?
Prospective parents should consider the ethical implications, the legal status in their country, the potential risks and costs involved, as well as their personal motivations and societal implications. Consulting with a fertility specialist and an ethical advisor is recommended to make a well-informed decision.