Explore the complexities of IVF, including costs, emotional impacts, health risks, success rates, and ethical concerns in our comprehensive guide.Navigating the complexities of starting a family, many couples and individuals turn to in vitro fertilization (IVF) as a beacon of hope in their journey toward parenthood. While IVF presents a significant scientific advancement with the potential to fulfill dreams of having a child, it also carries a set of challenges that are less frequently discussed. This blog post delves into the lesser-known drawbacks of IVF, providing insights into the financial, emotional, and ethical landscapes of this popular fertility treatment. From the daunting expense and low success rates to the potential health risks for both mother and child, and the web of emotional stress and ethical dilemmas it can weave, we aim to shed light on the crucial aspects prospective parents must consider. Understanding these cons is essential for making informed decisions in the emotionally charged and complex process of IVF.
Expense of IVF Treatment
The expense of In Vitro Fertilization (IVF) is notably one of the most daunting aspects for many couples struggling with infertility. The treatment is renowned for being costly, with expenses varying widely depending on location, individual clinic rates, and the specific circumstances of the patient. Generally, a single IVF cycle can cost anywhere from $12,000 to $25,000 in the United States, and this price can increase with additional cycles or if supplementary treatments are necessary.
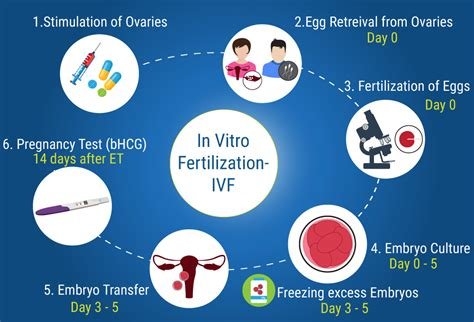
One major factor contributing to the high cost is that the process often requires multiple cycles before achieving a successful pregnancy. Each cycle involves numerous steps, including ovarian stimulation, egg retrieval, fertilization, and embryo transfer, each accruing separate costs for medications, medical interventions, and professional fees. Additionally, many couples face the need for pre-treatment diagnostics and post-treatment follow-ups, further increasing the financial burden.
Moreover, most health insurance plans do not cover the full cost of IVF treatment, and coverage varies significantly by plan and location, leaving many without sufficient financial support. This lack of comprehensive insurance coverage necessitates that many individuals and couples must pay out of pocket, which can lead to significant financial strain and requires careful financial planning and often substantial personal savings.
In light of these factors, the expense associated with IVF treatment remains a significant barrier for many, affecting accessibility and adding emotional and financial stress to the challenges of dealing with infertility.
Emotional Stress and Anxiety
In Vitro Fertilization (IVF) is a complex series of procedures used to aid in the conception of a child for couples facing fertility problems. Despite its success and widespread acclaim as a beacon of hope for many aspiring parents, the emotional stress and anxiety associated with the process can be significant and deserves consideration.
The emotional stress experienced during IVF is multifaceted, often beginning with the pressure of high expectations and the financial burden of the treatment. As couples navigate the demanding schedule of doctor’s appointments, tests, and procedures, the emotional toll can deepen. The use of hormonal treatments, which can have psychological side effects, only adds to the complexity of the emotions involved.
Moreover, the uncertainty and the typical multiple cycles required to achieve a successful pregnancy contribute significantly to anxiety. Each cycle of IVF can be a rollercoaster of hope and disappointment, compounding stress and creating emotional strain not just on the individual undergoing treatment but also on relationships.
Counseling and support groups for those undergoing IVF treatments can play a crucial role in managing emotional stress and anxiety. These resources offer a platform for sharing experiences and strategies for coping with the emotional challenges posed by IVF, fostering a supportive community to navigate this challenging journey.
Health Risks for Mother and Child
In vitro fertilization (IVF) is widely regarded as a beacon of hope for many aspiring parents struggling with fertility issues. However, like any medical intervention, IVF comes with its own set of health risks for both mother and child. Understanding these risks is crucial for anyone considering this treatment option.
For the mother, the process of IVF often involves the administration of synthetic hormones to stimulate the ovaries to produce multiple eggs. This process, known as superovulation, can lead to a condition known as ovarian hyperstimulation syndrome (OHSS). OHSS can be a serious health concern, causing symptoms ranging from mild abdominal discomfort to severe and life-threatening complications.
Additionally, IVF increases the risk of multiple pregnancies (twins, triplets, etc.), which significantly elevates the chances of premature birth and low birth weight. These outcomes not only pose a health risk to the infants but also to the mother, as carrying multiples often leads to complications such as gestational diabetes and preeclampsia.
The health risks for the child born via IVF have also been the subject of much scientific study. Research suggests that IVF may be associated with a small increase in genetic abnormalities and congenital malformations. Moreover, studies indicate a slight elevation in the incidence of rare imprinting disorders among IVF-conceived children compared to those conceived naturally.
While the majority of IVF procedures result in healthy babies and mothers, it is important for prospective IVF participants to fully understand and carefully consider the health risks involved. Consulting with healthcare providers to assess personal health factors and potential risks can aid significantly in making an informed decision about undergoing IVF treatment.
Low Success Rates of IVF
In Vitro Fertilization (IVF) is a widely discussed fertility treatment which involves the combination of an egg and sperm outside the body. Despite its popularity and scientific advancements, IVF carries a relatively low success rate which can be a major concern for many couples trying to conceive.
The success rate of IVF depends on a variety of factors including age, the cause of infertility, and lifestyle. However, statistically, the success rates are not as high as one might hope. For women under 35, the success rate of IVF is approximately 40%, but this rate dramatically decreases as age increases. By the age of 40, the success rate drops to 11-15% and continues decreasing thereafter.
This low success rate can lead to multiple cycles of treatment which not only increase physical and emotional stress but also heighten financial burdens. Each unsuccessful cycle can intensify feelings of frustration and hopelessness, impacting all areas of a couple’s life.
Furthermore, as clinics often promote their most successful cases, couples might have inflated expectations and are not fully prepared for the possibility of failure. This can lead to a significant emotional toll when the outcomes do not meet the expectations set by these highlighted success stories.
It is essential for couples to have realistic expectations and a clear understanding of all possible outcomes before embarking on what can be an emotionally and financially exhausting journey through IVF.
Ethical and Religious Concerns
IVF (In Vitro Fertilization) brings about significant ethical and religious concerns that often lead to debates across various communities. One major issue is the question of the status of the embryos used in IVF. From a religious standpoint, some argue that life begins at conception, and therefore, treating embryos as mere tools or objects might contravene certain moral and ethical principles. For instance, in many religious beliefs, the creation and destruction of embryos for scientific purposes can be seen as disrespect for life.
Another concern involves the methods involved in IVF, such as egg and sperm donation. These methods can raise issues about lineage and parental rights. Many religious doctrines have strict views about marital fidelity and biological lineage, and techniques that involve third parties may be problematic. This includes the use of donor eggs, donor sperm, or surrogates which can complicate the child’s understanding of parentage and heritage.
Furthermore, some faith traditions have concerns over selective breeding practices, such as choosing embryos based on preferred traits or genetic screening. These practices can lead to ethical dilemmas revolving around eugenics and the idea of “designer babies,” which may prioritize certain characteristics over others, potentially leading to societal divisions or inequalities.
Lastly, several ethical theories emphasize the potential exploitation of women, particularly concerning egg donation and surrogacy. The procedures for egg retrieval can be risky and burdensome, and the economic incentives can exploit economically disadvantaged donors. Critical voices argue that such practices commodify women’s reproductive capabilities, which poses profound ethical and humanitarian issues.
Overall, the ethical and religious concerns associated with IVF treatment are challenging and diverse, underscoring the need for ongoing dialogue among ethical theorists, religious leaders, and the medical community to ensure that respects for beliefs and ethical standards are maintained.
Frequently Asked Questions
What is In Vitro Fertilization (IVF)?
In Vitro Fertilization (IVF) is a medical procedure whereby an egg is fertilized by sperm in a laboratory dish. Once the egg develops into an embryo, it is then transferred to the uterus with the goal of achieving a successful pregnancy.
What are some common disadvantages associated with IVF?
Common disadvantages of IVF include its high cost, the potential for multiple pregnancies, emotional and physical stress, and the risk of ovarian hyperstimulation syndrome.
Why is IVF often considered a costly procedure?
IVF is considered costly due to the need for multiple appointments, sophisticated medical technologies, specialized medications, and sometimes, multiple treatment cycles to achieve a successful pregnancy.
Can IVF increase the risk of multiple pregnancies?
Yes, IVF can increase the risk of multiple pregnancies if more than one embryo is transferred to the uterus. This can lead to complications such as preterm labor and increased medical risk for both the mother and the babies.
How can IVF contribute to emotional stress?
IVF can be emotionally stressful due to the uncertainty of treatment outcomes, the hormonal effects of fertility drugs, and the physical and financial strains involved in the process.
What is Ovarian Hyperstimulation Syndrome (OHSS) and how is it related to IVF?
Ovarian Hyperstimulation Syndrome (OHSS) is a medical condition that can occur when the ovaries are overstimulated during the fertility medication phase of IVF. It can lead to painful, swollen ovaries and, in severe cases, more serious symptoms such as abdominal pain and shortness of breath.
Are there long-term health risks associated with IVF for the child or the mother?
Research is ongoing regarding the long-term health risks of IVF. While some studies suggest possible increased risks of certain health issues for both the child and the mother, definitive long-term effects are still being studied to establish a clearer understanding.