Explore artificial insemination and IVF, their processes, pros, cons, success rates, and costs to make informed fertility treatment choices.Navigating the world of assisted reproductive technologies can be an overwhelming journey for many aspiring parents. Two of the most popular methods that often come into consideration are Artificial Insemination (AI) and In Vitro Fertilization (IVF). Each approach offers distinct processes, benefits, and challenges that cater to different needs and circumstances. In this blog post, we’ll delve into the intricacies of both methods—starting with understanding the technical processes involved in AI and IVF, exploring their advantages and limitations, examining their success rates, and finally, comparing their costs. This comprehensive guide aims to equip you with the necessary information to make an informed decision on which option might be the best path toward parenthood for you.
Artificial Insemination: Understanding the Process
Artificial Insemination (AI) is a medical procedure used to treat infertility that involves directly inserting sperm into a woman’s uterus, cervix, or fallopian tubes. The primary goal is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization.
The process begins with the selection of sperm, which can be from the woman’s partner (partner insemination) or a donor (donor insemination). Before the insemination procedure, the sperm might undergo a process known as sperm washing which increases the chances of fertilization by removing chemicals in the semen that may cause adverse reactions in the uterus.
The timing of the insemination is critical and is usually coordinated with the woman’s ovulation cycle. Ovulation is monitored using ultrasound or blood and urine tests to ensure the best possible timing. In some cases, women may also be given medications to stimulate ovulation.
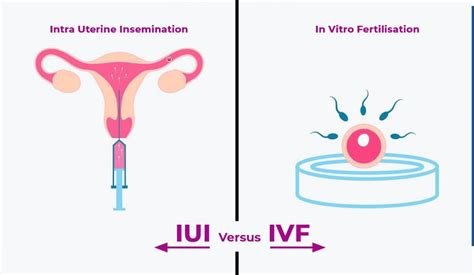
There are mainly two methods of AI: Intrauterine Insemination (IUI) and Intracervical Insemination (ICI). IUI involves placing sperm directly into the uterus, thus bypassing the cervix and increasing the number of sperm cells that reach the fallopian tubes. ICI, on the other hand, is a simpler technique where sperm is inserted into the cervix.
Artificial Insemination is considered a less invasive and more affordable option compared to other reproductive technologies like In Vitro Fertilization (IVF). It is commonly recommended for couples dealing with male infertility issues, such as low sperm count or motility, or where the source of infertility is unexplained.
In Vitro Fertilization: A Detailed Explanation
In Vitro Fertilization (IVF) is a medical procedure that aids in the conception of a child when natural or alternative methods of conception have not succeeded. It involves several key steps that each play a crucial role in the ultimate success of the procedure.
The initial step in IVF involves stimulating the woman’s ovaries with hormones to produce multiple eggs, rather than the single egg that typically develops each month. This is known as ovarian hyperstimulation. Doctors monitor this process through blood tests and ultrasound examinations to ensure optimal egg development and to determine the best time for retrieval.
Once the eggs are ready for retrieval, they are carefully collected from the ovaries using a minor surgical procedure, typically performed under sedation, to minimize discomfort. This process is conducted via a needle passed through the vaginal wall under ultrasound guidance, which aspirates the eggs and fluid from each follicle.
Following egg retrieval, the next critical phase is egg fertilization. The collected eggs are combined with sperm in a laboratory setting. This sperm may come from a partner or a donor. In some cases, where sperm quality or numbers are a concern, intracytoplasmic sperm injection (ICSI) may be employed, where a single sperm is injected directly into an egg to enhance fertilization chances.
After fertilization, the eggs develop into embryos. Embryologists monitor the embryos to choose the healthiest ones for transfer. The selected embryo or embryos are then transferred into the woman’s uterus. This procedure is less invasive and is done under ultrasound guidance to ensure the correct placement of the embryos within the uterine cavity.
Following the transfer, the patient typically remains in rest for a short period before continuing with their daily activities. Blood tests and possibly ultrasound scans are conducted approximately two weeks later to determine if implantation occurred and pregnancy has begun.
The whole process of IVF can be emotionally and physically demanding, but it has been a beacon of hope for many couples desiring to have a child. Advances in medical technology continue to improve the success rates of IVF treatments, making it a viable option for many families worldwide.
Pros and Cons of Artificial Insemination
Artificial insemination is a medical technique that can help individuals or couples conceive when they are facing difficulties with natural conception. Understanding the pros and cons of this technique is crucial for anyone considering this option.
Pros of Artificial Insemination
- Inclusivity: This procedure opens the door for many individuals, including single women, LGBTQ+ couples, and those with infertility issues, to conceive a child.
- Less Invasive: Compared to other reproductive technologies such as in vitro fertilization (IVF), artificial insemination is less invasive. It involves placing sperm directly into a woman’s uterus during her ovulation period, making it a simpler and less physically demanding process.
- Cost-Effective: Generally, artificial insemination is more cost-effective than IVF. This can be a crucial factor for many people when considering fertility treatments.
- Shorter Preparation Time: The preparation for artificial insemination is relatively short compared to IVF, which requires extensive hormone treatments and egg retrieval procedures.
Cons of Artificial Insemination
- Lower Success Rates: Compared to IVF, artificial insemination generally has lower success rates, particularly in older women or those with certain medical conditions.
- Multiple Births: While less common than with IVF, there is still a risk of multiple births with artificial insemination, especially if fertility drugs are used to increase the number of eggs produced.
- Legal and Ethical Issues: There can be legal and ethical issues to navigate, particularly concerning donor sperm and the rights of all parties involved.
- Emotional Strain: Despite being less invasive, the process can still be emotionally taxing, with cycles of hope and disappointment that impact emotional wellbeing.
Success Rates of In Vitro Fertilization
The success rates of In Vitro Fertilization (IVF) have been a crucial metric for couples considering this form of assisted reproductive technology. IVF involves the process of extracting eggs, retrieving a sperm sample, and then manually combining an egg and sperm in a laboratory dish. The embryo or embryos are then transferred to the uterus. A number of factors influence the outcome, including age, cause of infertility, and lifestyle factors.
According to recent studies, the average success rate of IVF falls around 30% to 35% per cycle, though this can vary significantly. For women under the age of 35, the success rate can be as high as 40-45%. This rate decreases as the age increases, with significantly lower success rates noted in women over the age of 40. The use of donor eggs, particularly from younger women, can increase these rates.
The success rates are also influenced by the clinic’s expertise and the specific technologies they use. Innovations like blastocyst culture and transfer, preimplantation genetic diagnosis (PGD), and intracytoplasmic sperm injection (ICSI) have helped to improve outcomes for many patients. Despite these advancements, the emotional and physical toll, along with the high costs of IVF, are significant considerations for those undergoing treatment.
It is also important for potential patients to understand that ‘success’ can be defined in several ways in the context of IVF; it could mean a positive pregnancy test, a pregnancy that leads to term, or the birth of a healthy baby. Each clinic may report their success rates differently and over different time frames, so it is crucial for patients to discuss these definitions with their healthcare provider to fully understand the data they are provided.
Cost Comparison: Artificial Insemination Vs In Vitro Fertilization
When considering fertility treatments, cost is often a significant consideration for many individuals and couples. In this section, we will compare the costs associated with Artificial Insemination (AI) and In Vitro Fertilization (IVF) to help those exploring their options understand the financial commitments involved in each procedure.
Artificial Insemination, also known as intrauterine insemination (IUI), is generally considered to be a less expensive option compared to IVF. The procedure involves directly inserting sperm into a woman’s uterus during her ovulation period. The costs for AI can vary widely based on factors such as the number of cycles undergone and whether or not additional treatments, such as fertility drugs, are needed. On average, a single AI cycle might cost between $300 to $1,000 in the United States. However, several cycles are often necessary to achieve pregnancy.
On the other hand, In Vitro Fertilization is a more complex procedure that involves extracting eggs and fertilizing them with sperm in a lab, before implanting the resulting embryos back into the uterus. IVF has a higher success rate per cycle compared to AI, but it also comes with a higher price tag. The cost of a single IVF cycle in the United States typically ranges from $12,000 to $17,000. This price can increase with additional cycles and if additional services such as genetic testing or egg donation are utilized.
It’s also important to consider that many insurance plans do not cover the full costs of fertility treatments, and the coverage terms can vary greatly. Potential parents must often pay significant out-of-pocket expenses. Additionally, the emotional and physical toll, as well as the time commitment for procedures like IVF, should be factored into the overall cost comparison.
In conclusion, while Artificial Insemination offers a more cost-effective option upfront, In Vitro Fertilization though more costly, potentially increases the chances of conception per cycle, which might be critical for many looking to start or expand their families. Each couple or individual must carefully weigh these financial aspects along with success rates, personal health circumstances, and emotional factors when choosing the right fertility treatment path.
Frequently Asked Questions
What is artificial insemination and how does it work?
Artificial insemination is a fertility treatment method that involves directly inserting sperm into a woman’s uterus, cervix, or fallopian tubes. The primary purpose is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization.
What is in vitro fertilization (IVF) and how is it performed?
In vitro fertilization (IVF) is a more complex procedure where eggs are collected from the ovaries and fertilized by sperm in a lab. The fertilized egg, or embryo, is then transferred to the woman’s uterus. This process can include monitoring and stimulating a woman’s ovulatory process, removing eggs from the ovaries, allowing sperm to fertilize them in a laboratory, and then transferring the embryos back into the uterus.
What are the main differences between artificial insemination and IVF?
The main difference lies in the technique and complexity. Artificial insemination involves inserting sperm inside a female’s reproductive tract, which is less invasive and less expensive. IVF involves manipulating both sperm and eggs outside the body, which is more complex, typically more expensive, and used often for more severe fertility issues.
Who might benefit from using artificial insemination?
Artificial insemination is often suitable for couples with unexplained infertility, minor male factor infertility, or women with cervical mucus problems. It is also a popular method for single women and lesbian couples wishing to conceive.
What are some reasons couples might choose IVF over artificial insemination?
Couples might opt for IVF if they have encountered issues like severe male infertility, blocked fallopian tubes, or previous unsuccessful fertility treatments including artificial insemination. IVF has a higher success rate per cycle compared to other forms of assisted reproductive technology.
Are there different types of artificial insemination?
Yes, there are several types of artificial insemination, the most common being intrauterine insemination (IUI), where sperm is placed directly into the uterus. Other types include intracervical insemination (ICI) and intratubal insemination (ITI), each differing in where the sperm is deposited within the female reproductive tract.
What are potential risks or side effects associated with IVF?
IVF can involve risks such as ovarian hyperstimulation syndrome (OHSS), where ovaries swell and become painful, multiple pregnancies which can pose risks to both mother and children, and potential emotional and psychological stress. There’s also a risk of ectopic pregnancy, where the embryo implants outside the uterus.