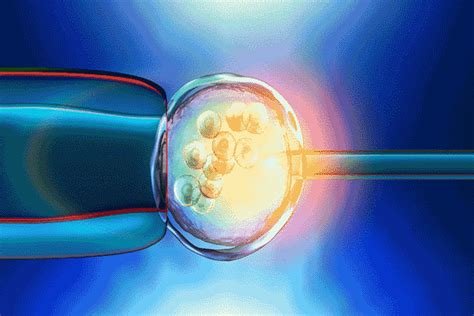
Explore key factors affecting IVF success: age impact, genetic factors, medical conditions, and lifestyle. Understand common reasons for IVF failures.In vitro fertilization (IVF) offers hope to countless couples grappling with infertility, but the journey isn’t always successful. Understanding why IVF fails can help manage expectations and pave the path toward future solutions. Various factors contribute to the likelihood of success or failure in IVF treatments, including biological, genetic, and environmental influences. This blog post explores some of the critical elements such as common reasons for IVF failure, the significant impact of age, underlying medical conditions, genetic factors, and how lifestyle and environment play pivotal roles. Arming yourself with this knowledge not only helps in making informed decisions but also prepares you for possible challenges along the path to parenthood.
Common Reasons for IVF Failure
In Vitro Fertilization (IVF) is a complex and emotional journey for many couples trying to conceive a child. Despite the advances in medical technology, IVF can sometimes fail, and understanding the common reasons behind this can help prospective parents manage their expectations and seek appropriate interventions.
Ovarian Response issues are one of the leading reasons for IVF failure. This occurs when a woman’s ovaries do not respond sufficiently to the hormone treatments meant to stimulate egg production. Poor ovarian response reduces the number of eggs available for fertilization.
Embryo Quality is crucial for the success of IVF. Embryos that exhibit poor morphology or have genetic abnormalities may not implant after transfer or may result in miscarriage. Advanced maternal age can further influence embryo quality, as older eggs have a higher chance of chromosomal anomalies.
Another important factor is the Endometrial Receptivity. An unresponsive or inhospitable uterine lining can prevent even the healthiest embryos from implanting. This can be due to various factors including fibroids, polyps, or hormonal imbalances.
Issues with the In Vitro process itself can also lead to failure. This includes errors in egg retrieval, embryo transfer, or in the handling and cultivation of embryos in the laboratory.
Lastly, Lifestyle factors such as smoking, excessive alcohol consumption, and obesity can negatively impact IVF outcomes. Environmental factors, such as exposure to certain chemicals and pollutants, are also thought to play a role in IVF success rates.
While IVF failure can be disheartening, understanding these common causes can help couples explore possible changes and alternatives in their pursuit of parenthood.
Impact of Age on IVF Success
The impact of age on IVF (In Vitro Fertilization) success is a crucial factor that couples and individuals must consider when planning to undergo this reproductive technology. Statistically, age is one of the most significant determinants of IVF success rates, influencing outcomes in several key aspects.
Firstly, the quality of eggs diminishes as a woman ages, particularly after the mid-30s. Older eggs can have higher rates of chromosomal abnormalities which may lead to decreased implantation rates and increased rates of miscarriage. This decline in egg quality directly correlates with a decrease in overall IVF success rates.
Moreover, the quantity of available eggs, or ovarian reserve, also declines with age. This decrease is measured by levels of Anti-Müllerian Hormone (AMH) and antral follicle count. Lower ovarian reserves can make it more challenging to retrieve a sufficient number of eggs for IVF procedures, which in turn can impact the number of embryos available for transfer.
Another age-related factor is the response to ovarian stimulation. Older women often require higher doses of medication to stimulate the ovaries, and even then, may still respond poorly as compared to younger women. This diminished response can result in fewer eggs being retrieved, which again decreases the chances of success.
Despite these challenges, it’s important for potential IVF candidates to have a comprehensive understanding of how age could impact their treatment. Consulting with fertility specialists who can provide tailored advice based on individual age-related factors is crucial. While age is a non-modifiable factor, understanding its implications can help in setting realistic expectations and planning the timing of IVF treatment more effectively.
Underlying Medical Conditions and IVF
In the journey toward conception through In Vitro Fertilization (IVF), various factors can influence the outcome, one of which includes underlying medical conditions of the partners involved. Understanding how these conditions can affect IVF success is crucial for couples considering or undergoing this reproductive technology.
Firstly, endometriosis is a significant medical condition that can impair the efficacy of IVF. This condition involves the growth of endometrial tissue outside the uterus, which can cause inflammation and scarring. These physical changes may not only hinder embryo implantation but also affect the quality of eggs and the overall environment of the uterus, thereby reducing the success rate of IVF procedures.
Another prominent condition is Polycystic Ovary Syndrome (PCOS), a hormonal disorder causing enlarged ovaries with small cysts on the outer edges. Women with PCOS typically experience irregular ovulation, which can complicate the synchronization of egg retrieval and embryo transfer, crucial steps in IVF. Moreover, PCOS is often associated with insulin resistance, which can adversely affect the quality of eggs.
Male factors, particularly poor sperm quality and quantity, also play a critical role in IVF success. Conditions such as varicocele, infections, or genetic disorders affecting sperm production can severely diminish the chances of successful fertilization and should be evaluated and treated before attempting IVF.
Moreover, uterine abnormalities, such as fibroids or polyps, can interfere with embryo implantation. The presence of these abnormalities might often necessitate surgical intervention prior to proceeding with IVF to enhance the chances of success.
Thyroid disorders, both hypo- and hyperthyroidism, can disrupt menstrual regularity and impair fertility. Adequate thyroid function is crucial for maintaining the hormonal balance necessary for successful pregnancy, making the management of these conditions essential before embarking on IVF.
Lastly, immune system disorders that lead to increased immune response can also impact implantation and pregnancy sustainability. Treatments to modulate the immune system might be considered for women who have experienced multiple unexplained IVF failures potentially linked to immune-related issues.
In conclusion, it is vital for couples considering IVF to undergo comprehensive medical screening to identify and manage any underlying medical conditions that could impede the success of the treatment. Collaborating closely with healthcare providers to address these issues can provide a clearer path toward achieving a successful pregnancy through IVF.
The Role of Genetic Factors in IVF Failure
In vitro fertilization (IVF) has revolutionized the way couples approach challenges with infertility. Despite its successes, not all IVF procedures result in pregnancy. Among various factors influencing IVF outcomes, genetic factors play a critical role in the potential failure of these treatments. Understanding how genetics can impact IVF is crucial for both medical professionals and potential patients.
Genetic abnormalities in the embryos themselves are one of the primary reasons for IVF failure. During the IVF process, embryos are created and then screened for viability before being transferred into the uterus. Abnormal numbers of chromosomes, known as aneuploidy, or specific genetic disorders can render an embryo nonviable. Even with pre-implantation genetic testing, some abnormalities might not be detected, leading to unsuccessful implantation or early miscarriage.
The genetic compatibility between the sperm and egg also influences the success of IVF. Specific genetic incompatibilities may prevent fertilization or hinder the embryo’s development. Additionally, the parental genetic background might contribute unidentified risks, potentially affecting the embryo’s development and the success of the IVF cycle.
Further, recent studies have suggested that the genetic makeup of the endometrium, or the lining of the uterus, can impact the success of implantation. A non-receptive endometrium, possibly influenced by genetic factors, may fail to support the embryo, preventing it from developing even if it is genetically healthy.
Advancements in genetic technology have led to more sophisticated methods of detecting potential genetic threats to IVF success. Techniques like Preimplantation Genetic Screening (PGS) and Preimplantation Genetic Diagnosis (PGD) offer hope in identifying genetic issues that could lead to IVF failure. However, these methods are not foolproof and sometimes do not capture all genetic nuances that could impact pregnancy outcomes.
As research continues, the role of genetic factors in the success or failure of IVF treatments remains a critical area of study. For those considering IVF, it is important to consult with genetic counselors and fertility specialists who can provide guidance based on the latest genetic insights and their implications for IVF.
Contributing Lifestyle and Environmental Factors
When discussing the challenges and outcomes related to In Vitro Fertilization (IVF), it is critical to consider the lifestyle and environmental factors that can significantly influence the success rates of these treatments. Various habits and exposures often play a more considerable role than initially anticipated.
Smoking and alcohol consumption are well-acknowledged lifestyle choices that negatively impact IVF success. Smoking has been linked to reduced ovarian reserve and poorer quality eggs, whereas alcohol can affect hormone regulation, which is crucial for successful IVF. Both direct and passive smoking are discouraged during IVF treatments.
Similarly, diet and obesity are pivotal. A balanced diet rich in antioxidants, vitamins, and minerals aids the body’s reproductive system. In contrast, obesity can lead to hormonal imbalances that might interfere with embryo development. Studies suggest maintaining a healthy body weight enhances the efficacy of IVF procedures.
Environmental toxins are another area of concern. Exposure to heavy metals like lead or mercury, and chemicals in pesticides or solvents, can disrupt reproductive functioning. Living in highly polluted areas or working in environments with high exposure to these substances can decrease the chances of IVF success.
Stress levels also play an essential role. High stress can lead to hormonal changes that might hinder IVF outcomes. Techniques such as mindfulness, yoga, or counseling are recommended to manage stress throughout the treatment process.
Considering these factors, those undergoing IVF treatments should consult their healthcare providers about optimizing their lifestyle choices and minimizing environmental exposures to improve their chances of success.
Frequently Asked Questions
What is in vitro fertilization (IVF)?
In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child. During IVF, mature eggs are collected (retrieved) from ovaries and fertilized by sperm in a lab.
What are common reasons for IVF failure?
Common reasons for IVF failure include poor embryo quality, inadequate endometrial lining, incorrect hormone levels, and the age of the woman undergoing the procedure. Additionally, lifestyle factors and genetic issues can play a significant role.
How does the age of the woman affect IVF success rates?
Age is a significant factor in IVF success. Women under 35 generally have higher success rates. As age increases, the quality and quantity of a woman’s eggs generally decrease, which can lead to lower success rates for IVF.
Can lifestyle changes impact the success of IVF treatments?
Yes, lifestyle factors such as smoking, alcohol consumption, excessive caffeine intake, and being overweight or underweight can negatively affect the success rates of IVF treatments by impacting egg quality, sperm quality, and hormone levels.
What role does embryo quality play in IVF success?
Embryo quality is crucial for IVF success. High-quality embryos have a better chance of implanting and developing normally. Factors that influence embryo quality include the age and genetic material of the donor eggs and sperm.
Is there a way to improve the chances of IVF success?
Improving IVF success can involve several approaches such as selecting an appropriate fertility clinic, choosing the right treatment protocol, using advanced technology for embryo selection, and making positive lifestyle changes. Preimplantation genetic screening (PGS) can also help select the best embryos for transfer.
What should couples do if they experience multiple IVF failures?
Couples experiencing multiple IVF failures should consider consulting with their fertility specialist to discuss possible reasons for the failures. Alternatives such as using donor eggs or sperm, surrogacy, or adoption might also be explored depending on the individual circumstances.