Explore the evolution and ethical debates on IVF. Delve into historical background, religious views, legal aspects, and the future of IVF ethics.In vitro fertilization (IVF) has revolutionized the prospects of parenthood for many, yet it also raises profound ethical questions that stir considerable debate across various sectors of society. Since its first successful application in 1978, IVF has not only been a beacon of hope for couples struggling with infertility but has also traversed complex moral landscapes. In this blog post, we explore the multifaceted ethical issues surrounding IVF. From its historical development, the ethical concerns posed in both theory and practice, to the varied religious standpoints and the legal frameworks governing its application, we delve into the intricate dimensions of IVF. What’s more, we will contemplate how evolving societal values and advancing technologies might shape the future of ethics in IVF, highlighting the continuous need for dialogue and policy adaptation in this ever-evolving field.
History of IVF
In Vitro Fertilization (IVF) has revolutionized reproductive medicine since its successful inception. The journey of IVF began in the late 1970s, marking a cornerstone in medical history. The first successful birth of a baby conceived through IVF, popularly known as the “test tube baby,” occurred in England in 1978. This groundbreaking event, involving the birth of Louise Brown, was led by Dr. Patrick Steptoe and Dr. Robert Edwards, paving the way for millions of births worldwide.
The development of IVF involved significant scientific challenges. Initially, researchers faced numerous biological and technological hurdles, including how to successfully fertilize an egg outside the human body and ensure its development into a healthy embryo. Overcoming these obstacles required innovative thinking and persistent experimentation.
Following its introduction, IVF technology rapidly advanced. Techniques such as cryopreservation, embryo screening, and intracytoplasmic sperm injection (ICSI) have since been developed, enhancing the effectiveness and accessibility of IVF. These advances have allowed many individuals and couples, including those with specific fertility challenges, to realize their dreams of parenthood.
In addition to technological advancements, the history of IVF includes expanding its ethical boundaries and societal acceptance. Initially met with skepticism and ethical concerns, IVF has now become a widely accepted practice in reproductive healthcare, though it continues to evoke debate regarding its implications and regulations.
Ethical concerns in IVF
In vitro fertilization (IVF) has presented new frontiers in the field of reproductive technologies since its inception. However, it has also spurred a variety of ethical concerns that continue to evoke diverse opinions among professionals, ethicists, and the public. One of the principal ethical concerns is related to the moral status of embryos. During IVF procedures, multiple embryos are often created, not all of which are transferred to a woman’s uterus. The decisions concerning the unused embryos—whether to dispose of them, freeze them for future use, or donate them for research—raise significant ethical questions about respect for potential human life.
Another key issue surrounds the rights and welfare of the child. IVF has made it possible for more individuals and couples, including those who are single or in same-sex relationships, to have children. This leads to questions about the rights of children to know their biological origins. Moreover, the use of third-party contributions such as sperm or egg donations, and surrogacy arrangements, introduces additional layers of complexity and potential for disputes regarding parenthood, disclosure, and the rights of all parties involved.
Additionally, the accessibility and high cost of IVF treatments also generate discussion about equality and justice in healthcare. IVF is an expensive procedure that is not always covered by insurance, potentially making it accessible only to wealthier individuals or couples. This disparity raises concerns regarding the fair distribution of medical resources and whether wealth should dictate one’s ability to have biological children.
Finally, the expansion of IVF and related technologies, such as preimplantation genetic diagnosis (PGD), prompts considerations about the possibility of ‘designer babies’. This term refers to the potential use of genetic selection to not only avoid genetic diseases but also to choose specific traits, which creates debates over human enhancement and the societal implications of such choices.
The ethical concerns surrounding IVF are complex and multifaceted, necessitating continued dialogue and thoughtful deliberation among healthcare providers, ethicists, policymakers, and society at large. As reproductive technologies evolve, so too must our approaches to addressing these crucial ethical issues.
Religious perspectives on IVF
In vitro fertilization (IVF) raises significant dialogue within religious communities, and perspectives vary widely among different faiths. Below, we explore the religious views from a few major religions regarding IVF practices.
Christianity‘s response to IVF can differ among denominations. The Roman Catholic Church opposes IVF because it separates conception from the natural act of marital union and often involves the disposal of embryos, which contradicts the belief in the sanctity of life from conception. However, some Protestant denominations are more accepting of IVF, particularly if it involves only the husband’s sperm and the wife’s egg without involving third-party donors.
In Islam, perspectives on IVF are also nuanced. IVF is generally permitted, but it must strictly involve the husband and the wife with no third-party donors, to maintain the genetic lineage and marital fidelity as commanded in the Quran. Surrogacy and the use of donor gametes are widely rejected.
Judaism typically embraces IVF within the frame of helping to fulfill the commandment to be fruitful and multiply, provided it is done within the bounds of Jewish law. Generally, Jewish law doesn’t recognize the pre-embryo as having full personhood and thus allows for some leniency in handling pre-embryos during IVF procedures.
Hinduism and Buddhism do not have central authoritative structures similar to those in other religions, which leads to varied interpretations. In general, both religions are more perceptive to medical interventions like IVF, viewing them as meaningful aids that help overcome suffering (in this case, the suffering of childlessness).
The ethico-religious discussions surrounding IVF continue to evolve as technology progresses, highlighting not just differences but also prompting dialogue among and within religious communities.
Legal regulations for IVF
In Vitro Fertilization (IVF), a form of assisted reproductive technology, has transformed the possibilities for many individuals and couples desiring to have children. However, the legal landscape governing IVF varies significantly from one jurisdiction to another, reflecting differing societal, ethical, and religious perspectives on the matter. Understanding these legal regulations is crucial for both medical practitioners and prospective parents.
In many countries, legal regulations for IVF focus on specific areas such as consent, the use of donor eggs and sperm, and the fate of unused embryos. For instance, laws may dictate how long embryos can be stored and the conditions under which they can be disposed. This directly influences the decisions and moral considerations faced by individuals undergoing IVF treatment.
In the United States, the legal framework for IVF is complex and varies by state. There are no federal laws specifically regulating IVF; instead, individual states may impose their own guidelines and statutes. This can include regulations on the number of embryos that may be implanted at one time, aiming to reduce the risks associated with multiple births.
In contrast, countries like the UK have centralized regulations under bodies such as the Human Fertilisation and Embryology Authority (HFEA), which oversees and inspects all clinics offering IVF. These bodies not only regulate the procedures but also address ethical questions like embryo research and genetic testing.
Furthermore, in some nations, legal frameworks address ethical concerns such as the anonymization of donor information, the rights of donor-conceived individuals to know their genetic origins, and the prohibition of gender selection, except where it is medically justified.
Each set of regulations reflects cultural, moral, and societal priorities that can significantly impact the accessibility and methods of IVF treatments available. As advancements in reproductive technologies continue, so too will the evolution of legal standards, requiring ongoing dialogue and adaptation to new ethical questions and scenarios presented by IVF.
The future of IVF ethics
In the realm of In Vitro Fertilization (IVF), ongoing advancements raise both hopes and ethical questions. As technology propels us forward, the future of IVF ethics is increasingly important—an arena filled with potential for transformative outcomes balanced by the need for thoughtful regulatory measures.
One of the primary ethical concerns is the enhancement of embryos. Scientists are now looking at ways not only to select embryos that are free from genetic diseases but also potentially to enhance genetic traits, which introduces questions about designer babies and socio-economic inequality. The ethical implications of such capabilities are vast, with arguments divided on the moral righteousness of genetic modification.
Another aspect is the accessibility and affordability of IVF treatments. As techniques improve and become more sophisticated, the cost of these treatments might increase, potentially making it less accessible to lower-income families. This raises ethical issues about equality and justice in healthcare, prompting a need for discussions about how these services can be made equitable.
Data privacy and security are also critical as IVF clinics collect and store large amounts of genetic information. Ensuring this data is protected against breaches is crucial to maintaining patient trust and respect for individual privacy.
Additionally, as the biological possibilities of IVF expand—potentially to even more controversial practices such as germline editing or cloning—the ethical landscape will need continual updating and regulation. The future of IVF ethics will have to evolve alongside these technologies, ensuring that moral considerations keep pace with capabilities.
Frequently Asked Questions
What is In Vitro Fertilization (IVF)?
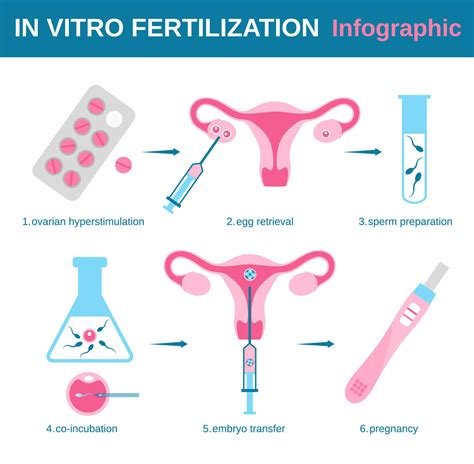
In Vitro Fertilization (IVF) is a medical procedure whereby an egg is fertilized by sperm outside the body, in a laboratory dish, and then implanted in a woman’s uterus.
What are the primary ethical concerns associated with IVF?
The primary ethical concerns include the status of unused embryos, the potential for selective breeding, the high costs associated with the procedures which may limit accessibility, and issues related to consent and exploitation.
How do different cultures view the ethical implications of IVF?
Cultural views on IVF vary widely; some cultures embrace it as a gift of science helpful for struggling parents, while others raise concerns about interfering with natural conception methods and the implications of such scientific intervention.
What role does religion play in the ethical debates surrounding IVF?
Religion plays a significant role, with various beliefs either supporting or opposing IVF based on interpretations of sacred texts regarding conception, the sanctity of life, and the definition of family and parenthood.
Is there a consensus among bioethicists about the use of IVF?
No, there is no universal consensus among bioethicists about IVF; opinions differ based on views about the moral status of embryos, reproductive rights, and the implications of reproductive technologies on society.
How are debates over IVF highlighting issues related to gender?
Debates often highlight issues such as the physical and emotional burden placed disproportionately on women, potential exploitation in egg donations, and pressures women may face regarding fertility and motherhood.
What legal frameworks exist to regulate IVF practices?
Legal frameworks vary significantly around the world, ranging from strict regulations and outright bans to more liberal approaches. These laws address aspects like consent, the number of embryos to be implanted, and the handling of surplus embryos.